|

Street Address: Mater Misericordiae Hospital, |
|
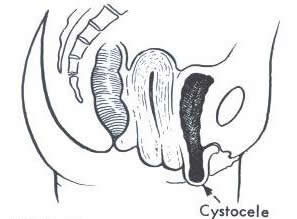
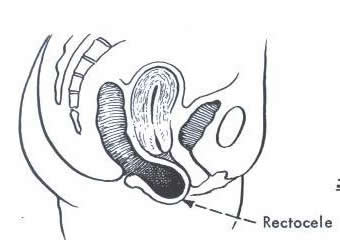
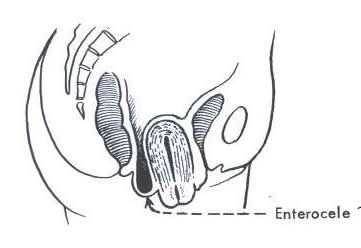
Pelvic organ prolapse
Symptoms: Common complaints with a prolapse are
|
||||||||||
Urogynaecology Education prepared by: Prof. A. Rane & A. Corstiaans CNC: January 2004. |